How do you collaborate through telehealth?
Telehealth has been on quite the journey since the days of Covid; increasingly used as a collaborative tool between healthcare providers. How can you collaborate even more via telehealth, particularly given the challenges it presents for podiatrists who need to be hands-on?
What we already know
Despite its clear limitations, telehealth has the potential to influence how podiatrists deliver care, particularly in remote and underserved areas where access to specialised services may be limited. Yet arguably, one of the most transformative aspects of telehealth lies in its ability to facilitate collaborative care models.
Firstly, what is the difference between shared care and collaborative care?
So, what is the difference between shared care models and collaborative care models? Especially given a shared care model is described as: “where there is joint responsibility for planned care that is agreed between healthcare providers, the patient and any carers they would like to engage.”
It may be reasonable to suggest there are little, if any, differences between the two models; since they are frequently used interchangeably in the literature.
However, through the example of telehealth, collaborative care enables a health care provider, such as a podiatrist, to work remotely with an on-site support person. This on-site support can help to facilitate the practical requirements of an appointment – such as removing a patient’s shoe, ensuring the camera angle is focused, aiding a patient to safely stand, or clearing the space for them to walk.
In this collaborative care context, the ultimate responsibility for the patient is not shared but instead maintained by the podiatrist.
How can the collaborative care model work in a telehealth context?
In the context of telehealth, this model can enable collaboration that may not otherwise be possible in-person.
Here are some ways this can work.
- Podiatrist + health professional: If another health professional is in the same location as a patient, the podiatrist can dial in remotely through video conferencing to guide the other professional to support the podiatrist’s component of the consultation.
- Podiatrist + family member/s: It is not uncommon for healthcare providers to ask a patient whether they wish anyone else to attend their telehealth session now that the location of the patient’s loved ones or support network is no longer a barrier.
- Podiatrist + patient: Shifting this approach further, the patient’s location can provide added insights during a video telehealth consult; compared to being in the clinic. If a podiatrist can see a patient’s living room for example, it may indicate some previously unknown social determinants of health and perhaps guide your decisions around social prescribing. Or you may see which available structures are nearby that can help support your session (such as a coffee table to lean on or a hazard to avoid). Sessions can become far more collaborative between the patient and podiatrist, increasing the relevance of treatment plans and the likelihood of self-efficacy.
- Podiatrist and colleague or other healthcare professional: Finally, the ability for telehealth to record sessions means that a podiatrist, with the patient’s permission, can share footage from the assessment or treatment session with other healthcare providers who can then work collaboratively across their separate areas of special interest. This collaboration extends to opportunities for mentoring and student learning, with new graduates for example likely to be more engaged through such practical learning opportunities.
What the research shows
Studies show that the impact of collaborative care models has potentially far-reaching effects such as targeting areas such as existing workforce challenges, low levels of engagement, and workplace longevity.
The Rural Doctors Network is close to completing an in-person collaborative care program that brings health professionals together from nearby areas who may not otherwise have the opportunity or means to collaborate. The goal being to address primary health care challenges in remote and regional NSW, such as recruitment and retention issues. Given the universal nature of these challenges, widespread learnings are still valuable no matter where your location.
Takeaways to bear in mind
The overarching takeaway from such explorations is a reminder that in this post-Covid-enforced isolation era we live in, telehealth still holds such potential for podiatrists, particularly when viewed through a collaborative lens.
There is scope to reach patients who may otherwise not be able to access podiatric services, such as those in remote or rural areas, or who are unable to physically attend an appointment and cannot access in-home care.
The first step is to think outside the box and consider how telehealth can help you to fulfill your role but in a different way; to see it as a truly collaborative tool that expands your patients’ horizons, your colleague’s engagement, and even your own networks.
Part 1 | The low-down on wearable devices + remote monitoring
With wearable devices, sensors, and remote monitoring gaining relevance; where do opportunities lie beyond tracking fitness, gait, and activity levels?*
*If you’re up to date on these technologies, consider devising your own healthtech solution; using some of the tips in Part 2 of this month’s special tech report.
With the tech landscape changing so quickly, it’s easy to get momentarily left behind – and it’s not uncommon for your patients to be the first to tell you about the latest wearable device or remote monitoring tool. While not an exhaustive summary, the following information recaps some of these latest developments.
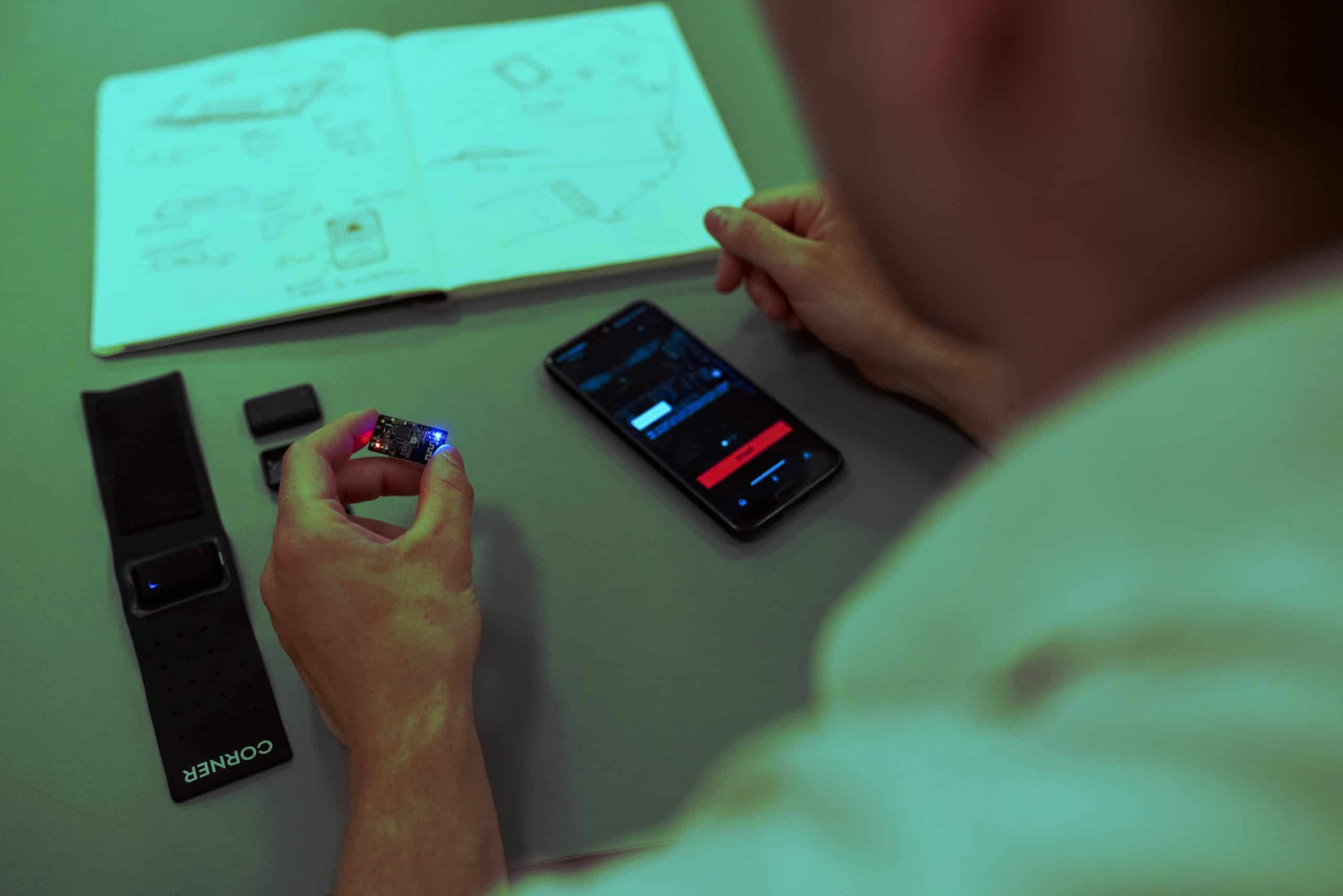
Firstly, what are wearable devices and sensors?
Wearable devices can include smartphone and smartwatch data. Sensors also fit within this category, yet they can also be attached to socks or directly on the skin inside a shoe, for example. A range of data can be collected from any of these technologies, such as temperature, heart rate, inflammation, or moisture levels.
There are many benefits to these kinds of metrics. Temperature monitoring can be useful in patients who have diabetes, whereas moisture detection can aid in tracking fungal infections or infections. This is just the tip of the iceberg however, no doubt you have come across countless other applications in your own experience.
What are remote monitoring devices?
These devices enable continuous monitoring of a patient’s foot health, outside of a clinical setting. For example, a patient may submit selfies of their foot via an app, such as MyFootCare, which was developed in Queensland. Other examples of remote monitoring include a UK start-up that is developing an at-home scanning device to detect oedema in patients who may be at risk of heart failure.
What are other examples of this technology?
- Balance and stability training devices: These devices are increasingly used in communities where people may be at high risk of falls, such as amongst people with diabetes and the elderly.
- Smart insoles: Often falling within the above category, but not always, these insoles can track pressure distribution, analyse gait, and even provide real-time feedback on a patient’s walking or running form. This technology is also being used in a range of populations, such as tracking falls-risk in people with Parkinson’s Disease and helping to prevent injury in people with diabetes.
- Footwear with built-in tech: Also connected to the above two categories, but not always, this technology covers shoes with integrated sensors to track movement or even sweat and other data.
- Pedometers and activity trackers: These wearables are probably what you come across most in your daily practice as a podiatrist, with patients sharing their activity and fitness statistics with you, alongside other valuable data.
What does the research say?
Extensive research exists in this area; these examples provide a starting point.
- Factors influencing Australian podiatrists’ behavioural intentions to adopt a smart insole into clinical practice: a mixed methods study
- The role of artificial intelligence technology in the care of diabetic foot ulcers: the past, the present, and the future
- The Potential Role of Sensors, Wearables and Telehealth in the Remote Management of Diabetes-Related Foot Disease
- Can a shoe-mounted IMU identify the effects of orthotics in ways comparable to gait laboratory measurements?
- Plantar pressure and falling risk in older individuals: a cross-sectional study
- Effects of supportive and minimalist footwear on standing balance and walking stability in older women
- Wearable sensors-based postural analysis and fall risk assessment among patients with diabetic foot neuropathy
Have an idea for a product?
Do you have an idea for a wearable device, software, app or other remote monitoring product? Part 2 in this month’s special report shares how to take a good idea for a podiatry product or healthtech solution – and turn it into something much bigger.

Part 2 | Have an idea for a healthtech solution?
Do you have an idea for a product, app, or piece of software that could help your patients (and many more beyond this?)* Then consider devising a scalable solution and taking the product development journey for yourself. Your unique exposure to patients’ challenges places you in the lead to create healthtech product solutions. Here are some ways to get started.
*If this world is a little new to you, consider reading Part 1 on wearables, scanners and remote monitoring solutions.
There are plenty of pathways into product development, here are some to consider.
#1 Read up on where the TGA sits
If you have a wearable device in mind, this rather dry but important first step offers a sensible way to explore if your concept may be TGA-compliant. This TGA resource provides a useful first step. (Hint: fast-track your search to page 5 if you’re short on time).
#2 Network with like-minded peers
There is a stack of networking opportunities available, which you can dive into by searching key terms like ‘tech start up + networking’. These include the following networks.
- With over 60,000 community members, The Start Up Network host pitch nights, networking events, remote networking, digital workshops and mentoring opportunities across Australia.
- Annual events like the Digital Health Fest are certainly worth considering. Digital Health Fest is Australia’s biggest digital health transformation event, attracting 4000 attendees and featuring the most innovative healthcare and healthtech leaders, pitch events, and a startup village.
- Don’t limit yourself to Australia. Check out global networking events such as StartUp Grind which takes place in the US and is a two-day event with plenty of opportunities for information sharing and networking. Or join online forums and remote communities such as CoFounders Lab (useful if you’re looking for a co-founder to help propel your idea forward).
#3 Explore funding and collaboration opportunities
Investors are ready to invest in your product or idea – provided you know how to pitch it well, your idea makes a difference, and it gives a great potential return on investment.
Here are some avenues to explore in this space.
- Entities like MTP Connect host an online searchable directory that lists funding opportunities alongside services that offer support in product development.
- The Biomedical Translation Bridge can help to fund and nurture early stage health and medical research ventures through to proof-of-concept stage. From there, your product or tech concept has the potential (and all-important exposure) to attract further capital and support.
- The Giant Leap Fund is Australia’s first venture capital fund that is 100% dedicated to investing in impact startups – rapidly scalable businesses that blend financial returns with real and measurable social and environmental benefits.
- Check out MedTech Actuator which supports MedTech innovators to commercialise niche ideas or genuinely new, hard-to-come-up-with, scientific discoveries that can “change the face of healthcare”.
- FLEDGE Innovation Labs is an independent enterprise that provides low-cost access to collaborative working spaces, laboratory facilities, scientific equipment, and business support. This is backed up by “an extensive network of experienced advisors and mentors from some of Australia’s most respected research institutions, service providers and multinational healthcare companies”.
- Universities can provide the structure of a start-up hub or an incubator program to support you on your journey, particularly if it is active in the healthcare space. Chat to your local university or search through directories to point you in the right direction.
Give it some thought
Podiatrists are already making gains in this space, and there’s no reason you can’t be next.
Why? Because you know where the current knowledge gaps exist when assessing or treating patients, and perhaps you have the seed of an idea that could help to bridge this gap. Not only could your concept ultimately benefit patients, but this added visibility can help to enhance the entire podiatry profession.
The Travelling Pod in Mexico | Part 3
The Travelling Pod shares this moving case study from the streets of Mexico, while also explaining how he made an ankle-foot orthotic out of recycled plastic cola bottle caps.
Follow David’s adventures and watch videos of his daily interactions at The Travelling Pod on YouTube.
Working on the street at the underpass next to the train tracks known as the vias, I saw a man amongst all the passing migrants, sitting down and wearing a bandage. At this time, I had Spike a Mexican volunteer of Amigos del Tren organisation, helping me to translate. Spike told me that this man from Honduras had a horse accident four years ago, injuring his left hip.
Initial impressions
The man’s gait was significantly affected, with an obvious weakness to his left leg to the foot causing a noticeable drop foot as if it were dead weight. He would load his body weight to his non-affected right hip and leg muscles to be able to complete the swing phase of his affected foot. He complained of muscle pain in his non-affected right gluteal muscles and feels unstable when he walks.
On observation and palpation when I rolled up his jean pants, he had significant muscle atrophy from his left leg down to his foot. He was unable to move his left affected foot into dorsiflexion compared to his normal moving right foot. His right foot presented with crawled toes in an attempt to grip the ground for stability compensating for his unstable left leg and foot. He had a significantly thick callus on his right lateral heel, complaining that it gets sore when he walks for a long time. Also, callus build-up on his right medial 1st inter-phalangeal joint because he pushing with medial angular propulsion due to a weak propulsive lever.
It was clear he had significant nerve damage as a result of his hip injury, also I was not able to detect 10 grams of pressure on his distal toes. Situations like this are sad because there is not much I can do for him to solve his problem; he needs to see a specialist for further investigation. However, I CAN DO SOMETHING to make his experience more comfortable.
Initial interventions
He was wearing flexible running shoes that were not broken thankfully (which is uncommon amongst passing migrants) but not suitable for his unstable foot. Unfortunately, I did not have any donated supportive shoes available to trade him, but at least he found his shoes comfortable to wear. I decided to use prefabricated orthotics that were donated generously and organised by Mona from Club Warehouse in Sydney Australia.
Also, I added an arch cookie slightly grinded down with my Dremel for extra support since the man had a high arch in his non-affected right foot during weight bearing. I recycled thongs/flip-flops to use the material as a minimal varus wedge to offload the 1st IPJ loading. I covered the orthotic with a 2mm EVA covering for comfort.
Since his left affected hip level was higher anteriorly and posteriorly during weight bearing, I felt comfortable adding a valgus lateral wedge to his heel to offload his high-impact area. I removed a lot of his thick callus to make his walking experience more comfortable. He felt comfortable and more stable in his walking, and he appreciated my efforts by giving me a hug.
Further intervention
Two mornings later, I woke up with an idea that interrupted my sleep.
I had an idea of making the man an ankle-foot-orthotic (AFO) out of recycled plastic Coke bottle caps. He needed an AFO to help his walking to avoid dragging his foot and significantly loading his right hip and leg muscles. I had never done this but it was an experiment that I was excited to try to hopefully bring him greater comfort and mobility. I brought the man into the Amigos del Tren center earlier than their operating hours (unfortunately, I got in trouble for it).
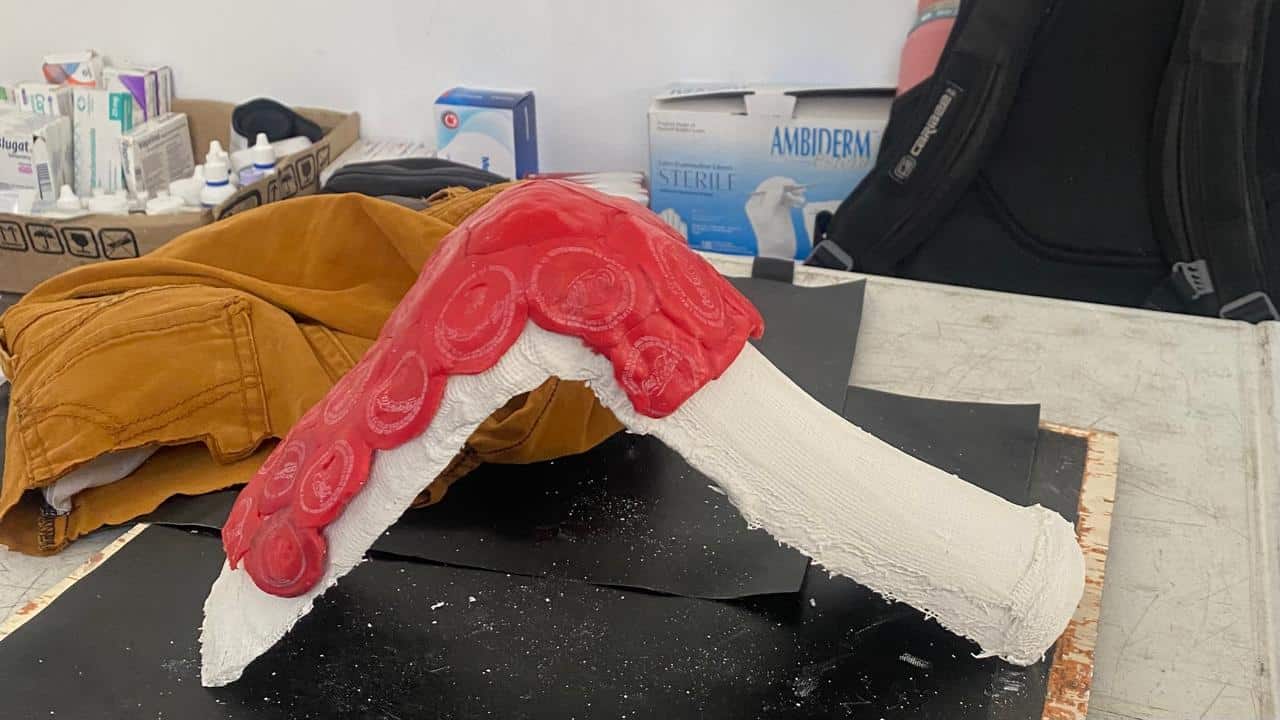
I cast his foot with his orthotic held in place with a bandage using plaster, and his foot held into a 90-degree dorsiflexed position. Then, I used my sandwich press to melt Coke bottle caps and laid the hot plastic over the cast. I continued this process until I had covered the majority of the plaster. As you can imagine, it was hard to mold without suitable gloves or the correct equipment.
I was able to make the desired shape and used my Dremel to shape it and flatten it so it could fit into his shoe appropriately. This project took half a day to complete, and continual trials on his foot. Lastly, I had glued 2mm EVA on the inside of the AFO where his Achilles tendon is.
The AFO was definitely not perfect, the biggest problem was the posterior shape not fitting inside his shoe. I had to continue to grind and fill weak spots with melted plastic bottle caps to provide more durability. I had to provide a 4mm hard EVA innersole under his orthotic for his non-affected right foot because the AFO raised him higher. He felt comfortable walking with the AFO and extra innersole (right foot), also using a bandage to lock his leg to the AFO.
The next day he was not using the AFO and I asked why. He had changed shoes (thrown out his previous pair) for a more supportive casual shoe (donated by a visiting church group) but the toe box was too shallow for the AFO and orthotic.
Patient feedback
I cut the orthotic to make it a ¾ length and that fitted better, and with a little more grinding, the AFO and orthotic felt comfortable. Using a translator, I asked for his honest feedback reassuring him that he would not offend me with my first AFO trial. He complimented the device and saw him wearing it for the day, and other days he has not worn it. He knows he can just use the prefabricated orthotics if the AFO bothers him, but he said he uses it when he walks a lot – honestly, I am not too sure but I did give him my best.
Follow The Travelling Pod
YouTube: The Travelling Pod
Instagram: www.instagram.com/the_traveling_pod/
Website: www.TheTravelingPod.com

How to encourage patient-reported measures
Patient reported measures provide a useful lens to better understand how a patient views their health and wellbeing. Podiatrists who access this data can support a more informed treatment approach. Yet, knowing how or where to start can be the biggest stumbling block of all. Here’s the low down on what these measures are, why they matter, and how to collect them.
In healthcare, the focus is often on clinical outcomes and measures such as blood pressure, cholesterol levels, and tumour size. These measures are important in diagnosing and monitoring medical conditions and determining the effectiveness of medical treatments. Clinical measures provide critical information for healthcare providers to make decisions about medical treatments and interventions.
However, the patient’s experiences and outcomes are just as important as these clinical measures. Patient reported measures (PRMs) are a way to capture patients’ perceptions of their health and well-being. In this blog, we will discuss what PRMs are, why they are important, and how they are used in healthcare.
What are Patient Reported Measures?
Patient reported measures (PRMs) are tools used to assess patients’ health status and quality of life from the patient’s perspective. These measures are based on patient self-reporting and can include surveys, questionnaires, interviews, and other data collection methods. PRMs can provide valuable insights into patients’ experiences, including their symptoms, functional status, psychological wellbeing, and satisfaction with care.
There are two major types of patient reported measures:
1. Patient Reported Outcome Measures (PROMs):
Patient reported outcome measures are self-administered questionnaires or interviews that gather information directly from patients about the outcomes related to their health and wellbeing. These measures are designed to capture patients’ perceptions of their physical, psychological, and social functioning and can help providers get a more accurate picture of how a particular treatment is impacting their patients’ lives.
PROMs can also be used to assess the impact of medical treatments on specific populations, such as elderly patients or patients with chronic conditions. In these cases, PROMs can provide valuable information about the unique needs of these populations and help healthcare providers tailor their treatments to better meet these needs.
2. Patient Reported Experience Measures (PREMs):
Patient reported experience measures are tools used to gather information from patients about their experiences with healthcare. The objective of these measures is to give patients a voice in the assessment of the quality of care they receive and to improve the delivery of care by taking their perspectives into consideration.
PREMs can be used in various stages of the healthcare journey and are usually collected from patients via questionnaires, surveys, interviews, focus groups or patient portals or tools. They can cover a range of topics, including communication with healthcare providers, the physical environment of the healthcare setting and the overall quality of care received.
Why are Patient Reported Measures important?
PRMs are important because they allow healthcare providers to understand the patient’s perspective and tailor care to meet their unique needs. By capturing patients’ experiences, PRMs can help identify areas where care can be improved, as well as track progress over time. In addition, PRMs can help providers communicate with patients about their health and empower them to make informed decisions about their own care.
PRMs can also be used for research purposes, allowing researchers to study the patient experience and evaluate the effectiveness of interventions. By incorporating PRMs into research studies, researchers can capture the patient perspective in a standardised and systematic way, which can help improve the quality of research.
Under a value-based care delivery model, improving outcomes and experience is one of the best ways to show you are partnering with patients. It is also how you demonstrate that you are delivering the outcomes that matter to your patients and will be the metric which determines your fee for value under a value-based model of care – that is, the value you are returning to your patients.
How are Patient Reported Measures used in healthcare?
PRMs can be used in a variety of healthcare settings, including primary care, specialty care, and hospital settings. In primary care, PRMs can be used to assess patients’ health status and identify areas where care can be improved. For example, a primary care provider might use a depression screening tool to assess a patient’s mental health status and determine if a referral to a mental health specialist is needed.
In specialty care, PRMs can be used to assess patients’ functional status and quality of life related to a specific condition. For example, a patient with rheumatoid arthritis might be asked to complete a survey about their pain, fatigue, and ability to perform daily activities.
In hospital settings, PRMs can be used to assess patients’ experiences of care. For example, patients might be asked to complete a survey about their hospital stay, including their satisfaction with the care they received, the quality of communication with their providers, and the cleanliness of the hospital environment.
How do I get started with Patient Reported Measures?
Measuring outcomes and experience is one of the easiest places to start your value-based health care journey.
It’s important not to create your own survey unless absolutely necessary as there are a lot of endorsed PROMs and PREMs surveys already available to use. Using an endorsed PROMs or PREMs survey ensures that the instrument has been scientifically validated and is reliable, valid, and responsive to changes in the patient’s health status. The use of endorsed PROM surveys also helps to ensure that the data collected is comparable across different healthcare settings and patient populations.
A good place to start looking for validated patient reported measurement surveys is to check with your professional association or relevant state or territory health department or visit the ICHOM (International Consortium for Health Outcomes Measurement) or Australian Commission on Safety and Quality in Health Care websites.
Patient reported measurement surveys can be undertaken using simple online survey tools or you may wish to use a specialist PROMs and/or PREMs software platform, that collects and analyses the data.
Do I have to use Patient Reported Measures in my practice?
Whilst there is not currently a mandate for Australian health care organisations to collect patient reported outcome or experience measures, health reform is coming in Australia which indicates that practices will need to start measuring the value they are delivering to their patients under a ‘pay for value’ model.
More information
For more information regarding the momentum and reform building towards the adoption of value-based health care in Australia, watch Patient Experience Agency’s free webinar: “Australian Health Reform: a guide for what it means for you and your practice”

Have you used the employee retention checklist?
In any workplace setting, maintaining a stable and engaged workforce is essential for sustaining productivity and fostering a positive organisational culture. Effective employee retention strategies play a pivotal role in achieving these objectives by ensuring that skilled and experienced employees remain committed to their roles within the business. Beyond simply reducing recruitment costs, they show a commitment to employee satisfaction and well-being, which in turn contributes to the long-term success and competitiveness of the organisation.
This article will focus on our Employee Retention Checklist, offering employers a practice resource.
Member-only full article access available at APodA’s Human Resources Portal.