
Endorsed-prescribing podiatrist and Medicines in Podiatry Special Interest Group member, Zahava Robinson of Bondi Podiatry draws from her own experience to discuss the updated guidelines for treating fungal infections.
As an endorsed-prescribing podiatrist, I’ve always aimed to stay updated on the latest treatment guidelines for fungal infection, while remaining conservative in my treatment where possible.
These guidelines do not change the way most podiatrists treat topical fungal skin infections, it reflects what podiatrists have already been doing in practice. Nonetheless, this article reflects my personal experience and understanding of the new guidelines and their practical implications for us in the field, particularly for endorsed prescribers.
These guidelines reiterate that topical antifungals are really quite safe, much safer than orals. Research exists to show that some topical treatment can be appropriate and safe during pregnancy, which is why these updated guidelines are so important.
When the Therapeutic Guidelines were updated to refine the recommended treatments for fungal infections, particularly tinea pedis, I believe it actually aligned more closely with what the majority of podiatrists were doing.
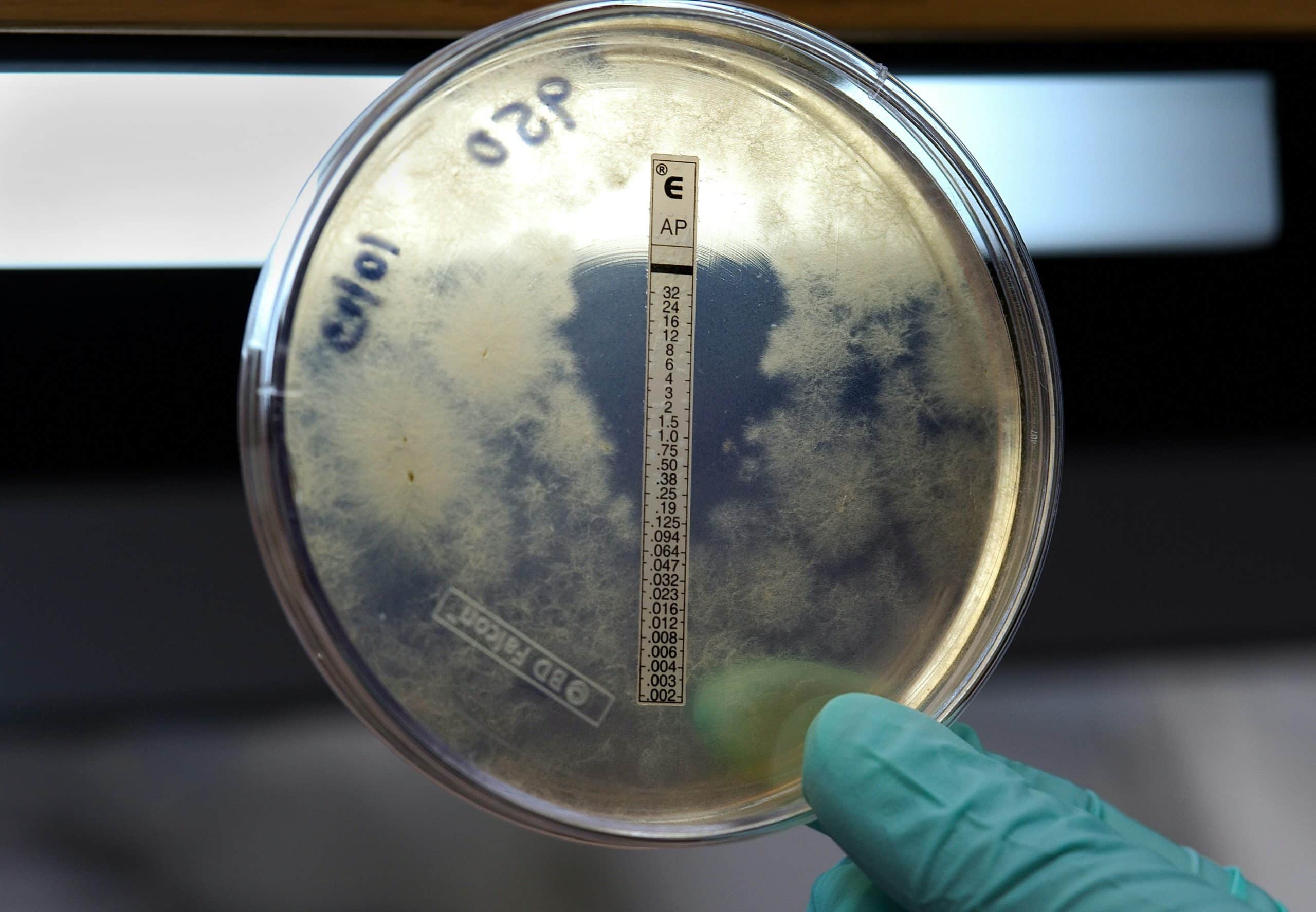
Importantly, the revisions distinguish between different types of tinea and specify when to use topical versus systemic treatments. The updated guidelines state:
Tinea is treated topically or systemically depending on its extent and location:
For endorsed podiatrists, the recommended management includes:
Griseofulvin is an option due to its ability to be crushed and taken with fatty foods, which can aid in its absorption. However, I hold concerns about certain antifungal medications such as this older medication. It’s becoming clear that these older treatments are less effective and have been largely replaced by newer, more effective options.
On that issue, one group of medications that I believe should be included more broadly is the azoles. Azoles are a class of antifungal medications with a broader spectrum of activity and different coverage. Their inclusion in our treatment arsenal could significantly enhance our ability to manage fungal infections more effectively.
The previous guidelines were quite rigid, advocating for oral antifungals as the primary treatment for tinea infections. This approach, though well-intentioned, had its drawbacks. In practice, I often found that topical treatments were effective for localised infections; a fact that wasn’t fully supported by the older guidelines.
In my practice, I’ve encountered numerous cases where oral antifungals were prescribed, but not always with the best outcomes. One notable example involved a young patient who had taken oral antifungals for three months. In this scenario we had to cease treatment in an otherwise health individual due to low total protein and low globulin which indicated liver damage until this was reviewed by his GP.
With the updated guidelines, we can more effectively use topical treatments for fungal infections, especially those confined to areas like between the fingers or toes. This shift is a significant improvement, allowing us to provide safer and more targeted treatment. I’ve always believed in the efficacy of topical treatments for these localised infections, and the new guidelines support this approach.
This change also allows for greater flexibility in our treatment plans. Instead of defaulting to oral medications, which carry risks of systemic side effects, we can now choose topical antifungals that directly address the infection without the same level of risk.
As podiatrists we know that topical antifungals remain a crucial part of treating surface-level infections. They work directly on the affected area, reducing systemic exposure and potential side effects.
I see topical treatments as similar to antibiotics in their specificity. Just as we select antibiotics based on the type of bacterial infection, we should choose antifungals based on the specific fungal pathogen and the infection’s location. This approach ensures that we provide the most appropriate and effective treatment.
In my experience, treating tinea often involves a bit of a process. Sometimes, the first medication we try isn’t the one that works as well as another medication might for a particular patient.
For instance, we might start with one topical or oral antifungal and see if it clears up the infection. If it doesn’t, we may need to switch to another medication. This process can be frustrating for patients, but it’s often necessary to find the most effective treatment.
I’ve had patients where we had to experiment with different oral treatments before finding one that worked well. It’s important to be patient and persistent because what works for one person might not work for another. In addition, there are terbinafine resistant infections in the community which is another factor to consider and further highlights the need for endorsed podiatrists to access oral azole antifungals.
Each case is unique, and sometimes it takes a bit of tweaking to get the best result, and I try to manage patient expectations around this issue as much as possible.
When it comes to treating tinea and other fungal infections, I’ve always emphasised that addressing the source of the infection is just as crucial as applying the medication, whether it’s topical or oral. I’m sure that being a podiatrist yourself, you are in full agreement, and together we acknowledge that our main challenge lies in patient education.
In my practice, I frequently encounter patients who, despite following their prescribed treatment regimen, continue to experience recurrent infections. Clearly, a more comprehensive approach is needed — one that includes not just medication, but also meticulous hygiene and lifestyle adjustments.
We need to emphasise to our patients that it is essential to consider the environment in which the infection thrives. We know that tinea fungi can persist in places like bath towels, bed sheets, and shoes. We also know that these items can harbour fungal spores and potentially reinfect the patient even after the infection seems to be under control.
I advise my patients to wash their bath towels, bed linens, and clothing regularly in hot water and with antifungal detergent if possible. Likewise, organic apple cider vinegar soaks can provide a helpful adjunct to traditional treatments, creating an unfriendly environment for fungal infections to flourish. This should not replace prescribed medications but rather complement them.
This practice helps to eliminate any residual fungi and prevent the reinfection cycle. Additionally, shoes, especially those that are worn frequently and in damp environments, should be cleaned thoroughly. I recommend airing them out regularly and using antifungal powders or sprays to keep them dry and free of fungi. Fungal infections also occur in moist warm environments and having moisture wicking socks (such as cotton or bamboo) and breathable footwear is a way to reduce the risk of recurrence.
It’s also important to educate patients about the role of personal items like nail clippers and razors, which should be disinfected regularly or replaced to avoid cross-contamination. By addressing these aspects, we can reduce the risk of reinfection and improve the overall effectiveness of the treatment.
It is important to acknowledge the link between fungal infections and genetics.
There is a susceptibility based on genetics, and the likelihood of repeated or prolonged treatment and the impact of oral prescription needs to be considered as these medications involve a level of risk.
I believe that the recent updates to fungal infection treatment guidelines represent a positive shift towards safer and more effective care. By recognising the value of various topical treatments and advocating for a broader range of antifungal options, these guidelines align better with clinical practices and patient needs.
As practitioners, it’s essential for us to stay informed about these changes and consider their implications for our practice. With the right knowledge and resources, we can offer improved care and achieve better outcomes for our patients in managing fungal infections.
Do you want to join the Medicines in Podiatry Special Interest Group? Find out more.
© Copyright 2021 The Australian Podiatry Association
